Email
info@lgsc.co.uk
Email
info@lgsc.co.uk
Phone
0203 312 6130
Location
The Lindo Wing, St Mary’s Hospital,
Praed Street, London W2 1NY
Pancreatitis means inflammation of the pancreas. In acute pancreatitis, the inflammation develops quickly, over a few days or so. The digestive chemicals (enzymes) that are made in the pancreas become activated within and start to 'digest' parts of the pancreas. It often goes away completely and leaves no permanent damage in most cases. In most cases, the inflammation is mild, symptoms settle within a week and pancreas fully recovers. However, in some cases, the inflammation quickly becomes severe. Parts of the pancreas and surrounding tissues may die (necrosis). Pancreatic enzymes and chemicals may get into the bloodstream and cause inflammation and damage to other organs in the body. This can lead to shock, respiratory failure, kidney failure and other complications. This can be a very serious situation, which can occasionally result in admission to the intensive care unit.
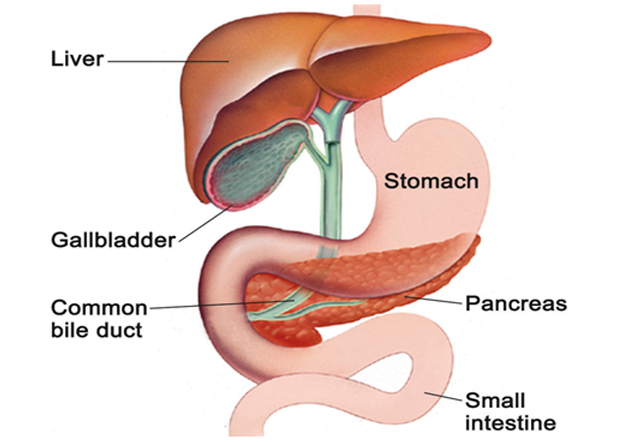
The pancreas is in the upper abdomen and lies behind the stomach and intestines. It makes a fluid that contains chemicals (enzymes) that are needed to digest food and hormones to control blood sugars. The enzymes are made in the pancreatic cells and are passed into tiny tubes (ducts) of pancreas. These ducts join together like branches of a tree to form the main pancreatic duct, which joins the bile duct carrying bile from liver and gall bladder before it opens into the initial part of the small intestine, called the duodenum, just after the stomach. The enzymes are 'activated' in the duodenum to digest food.
Most common causes of pancreatitis are gallstones and alcohol. A gallstone is formed from bile that flows from liver and gall bladder; pass through the bile duct and out into small intestine. Gallstones commonly contain lumps of fatty (cholesterol-like) material that has solidified and hardened. If they gets stuck in the bile duct or where the bile duct and pancreatic duct open into the duodenum, it can affect the chemicals (enzymes) in the pancreatic duct and trigger a pancreatitis. How alcohol actually triggers the inflammation in the pancreas is not clear. Symptoms typically begin about 6-12 hours after a heavy drinking session. In some people pancreatitis can develop even after a small amount of alcohol. In these people, ’sensitivity’ to alcohol develops in their pancreas. Other rare causes of pancreatitis include infection, high blood fat or calcium levels, abnormal structure of the pancreas, inherited from a parent (hereditary) and autoimmune, where body’s own immune system attacks the pancreas. Often, no cause is found, this is known as idiopathic pancreatitis.
Pancreatitis usually presents with central/upper abdominal pain. It usually builds up quickly (over a few hours) and may last for several days. The pain can become severe and is typically felt spreading through to the back. It is associated with being sick (vomiting), fever, feeling unwell, and abdomen may appear swollen. However, it is occasionally possible to have acute pancreatitis without any pain. This is more common if you have diabetes or have kidney problems.
If pancreatitis is suspected, the patient is admitted to the hospital. Blood tests are carried out and level of amylase and/or lipase, enzymes made by the pancreas, is checked. Although not 100% reliable, a high blood level of these enzymes strongly suggests that pancreatitis is the cause of your symptoms. An ultrasound or CT scan is usually conducted to check for cause and severity of pancreatitis.
The treatment depends on how bad the attack of acute pancreatitis is. Till the time inflammation settles, the following supportive measures can be provided to avoid complications from occurring:
Strong painkillers
A tube may occasionally also be passed down your nose into your stomach (nasogastric tube) to suck out the fluid from your stomach. This can be useful if you are vomiting a lot.
A nasogastric tube may also be passed into the stomach to feed you, as you will not be able to eat properly.
A 'drip' is needed to give fluid into your body until symptoms settle.
A catheter (this is a thin tube going into your bladder, which drains urine) is likely to be inserted so the doctors can monitor accurately the amount of urine you are passing.
Less commonly, complications develop and the situation can get very serious. Other treatments that may then be needed include the following:
Intensive care treatment. If you have a severe attack of pancreatitis then you will be monitored very closely in the intensive care unit.
A procedure to remove a blocked gallstone if this is found to be the cause.
Antibiotics if the pancreas or surrounding tissue becomes infected.
Surgery is sometimes needed to remove infected or damaged tissue.
An attack of acute pancreatitis may be a one-off event. One of the following may be relevant to prevent a recurrence, depending on the cause:
An operation to remove your gallbladder is usually advised if a gallstone was the cause.
If alcohol is the cause of pancreatitis, you should stop drinking alcohol altogether.
A high blood fat level (hyperlipidaemia) is sometimes the cause. This may need treating with medication.
A side-effect from some medication is a rare cause of acute pancreatitis. A change in medication may be needed if this is your cause of pancreatitis.

Please note, most insurance policies in the UK do not cover weight-loss surgery. However, we will do our utmost to provide the best package for you should you choose to have your surgery with us.
The contents on this site is for information only, and is not meant to substitute the advice of your own physician or other medical professional.